Healthcare Fraud Analytics Market Outlook:
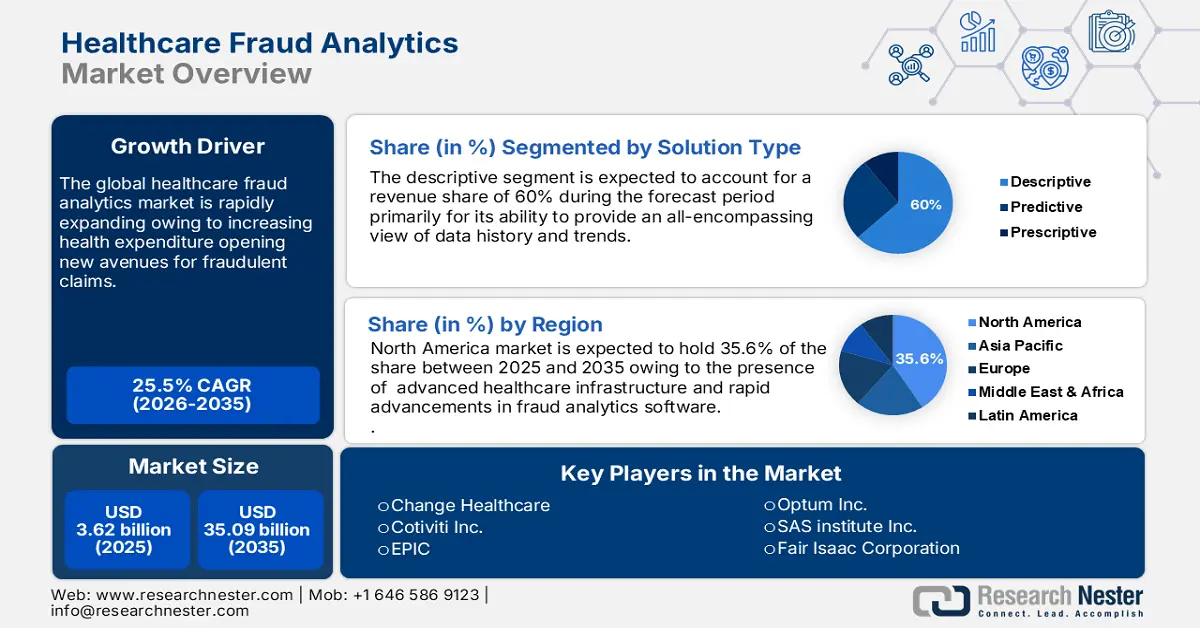
Healthcare Fraud Analytics Market size was valued at USD 3.62 billion in 2025 and is likely to cross USD 35.09 billion by 2035, registering more than 25.5% CAGR during the forecast period i.e., between 2026-2035. In the year 2026, the industry size of healthcare fraud analytics is assessed at USD 4.45 billion.
The crucial growth drivers that fuel the growth of the market are budding health expenditures that open avenues for fraudulent claims and thus make it imperative to adopt advanced analytics. Also, a wide acceptance of data analytics and AI in healthcare facilitates detecting and preventing fraudulent claims. Furthermore, regulatory pressures and compliance mandates fuel market growth as healthcare organizations strive to meet the standards. With the rising incidence of healthcare fraud associated with identity theft, billing errors, and the manipulation of a patient's medical records, the need for proactive detection rises and drives growth. Moreover, advances in machine learning and predictive modeling and the shift from pay-and-chase to enable real-time prevention of loss in financial fraud assist the market to be opportunistic.
Another significant reason for the market propels owing the growing demand due to IoT and cloud computing, real-time analytics, and visualization, the need for risk management and compliance solutions is growing, as value-based care and payment integrity. Thus, all these factors come together and form a compelling business case for healthcare fraud analytics and drive investments and innovation in the market. In August 2024, Medibuddy introduced Sherlock, a cutting-edge AI-enabled fraud detection system that allows for the real-time detection of medical reimbursements incorporated with artificial intelligence, machine learning, and data analytics.